日本科学家揭示肝炎或导致不同肝癌表型
原发性肝癌是全世界诱发死亡的第三大癌症。最近研究表示,特别是在亚洲,乙型或者丙型肝炎感染者更容易患肝癌。通过全基因组测序技术,日本科学家首次揭示了慢性肝炎感染对肝内细胞癌变的影响。这篇研究成果发表在最新的Nature Communications杂志。
肝癌有诸多分类,其中肝内胆管癌和肝细胞合并胆管癌由于在组织学上显示有不同程度的胆管上皮细胞分化,被定义为有胆管表型的肝癌(Liver Cancer displaying biliary phenotype,LCB)。LCB通常与肝细胞癌相比,侵入性更强,预后差。为了了解LCB的分子改变,研究人员对30个LCB肿瘤样品进行全基因组测序。作为比较,研究人员同时测序了另外60个常见肝细胞肿瘤样品,并详细分析其中一些样品RNA测序结果。
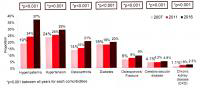
图片来自原研究论文。图片表示肝细胞癌(灰色点)与肝炎阳性的LCB(黑色点)是重合的,而肝炎阴性的LCB(蓝色点)却不相关。
令人惊讶的是,他们发现尽管肝细胞癌和LCB基因表达的模式不同,细胞内整体的突变模式竟是类似的-这主要出现在乙肝或者丙肝感染的患者。未有肝炎感染的患者基因突变模式却是不同的。这表明不同组织学类型的肝癌可能是从肝炎感染患者相同类型细胞衍生而来,比如肝祖细胞。
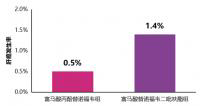
通过后续分析,研究人员识别了恶性LCB相关的几种重要的基因的突变,包括TERT启动子,染色质调节子 ( BAP1 ,PBRM1 和ARID2 ), 突触结构基因 ( PCLO ),IDH基因 和KRAS基因。KRAS和IDHs突变--通常与恶性肿瘤相关,被发现主要存在于未曾患慢性肝炎的癌症患者。
这项研究,主要表明慢性肝炎对LCB的基因突变类型的影响。通过这个分析,或许能帮助确认哪些LCB表型更接近肝细胞癌,哪些更类似于胆管癌。对于不同的LCB表型制定合适治疗方法。
DOI: 10.1038/ncomms7120
Whole-genome mutational landscape of liver cancers displaying biliary phenotype reveals hepatitis impact and molecular diversityAkihiro Fujimoto, Mayuko Furuta, Yuichi Shiraishi, Kunihito Gotoh, Yoshiiku Kawakami, Koji Arihiro, Toru Nakamura, Masaki Ueno, Shun-ichi Ariizumi, Ha Hai Nguyen, Daichi Shigemizu, Tetsuo Abe, Keith A. Boroevich, Kaoru Nakano, Aya Sasaki, Rina Kitada, Kazihiro Maejima, Yujiro Yamamoto, Hiroko Tanaka, Tetsuo Shibuya, Tatsuhiro Shibata, Hidenori Ojima, Kazuaki Shimada, Shinya Hayami, Yoshinobu Shigekawa, Hiroshi Aikata, Hideki Ohdan, Shigeru Marubashi, Terumasa Yamada, Michiaki Kubo, Satoshi Hirano, Osamu Ishikawa, Masakazu Yamamoto, Hiroki Yamaue, Kazuaki Chayama, Satoru Miyano, Tatsuhiko Tsunoda, Hidewaki Nakagawa.
Abstract
Intrahepatic cholangiocarcinoma and combined hepatocellular cholangiocarcinoma show varying degrees of biliary epithelial differentiation, which can be defined as liver cancer displaying biliary phenotype (LCB)。 LCB is second in the incidence for liver cancers with and without chronic hepatitis background and more aggressive than hepatocellular carcinoma (HCC)。 To gain insight into its molecular alterations, we performed whole-genome sequencing **ysis on 30 LCBs. Here we show, the genome-wide substitution patterns of LCBs developed in chronic hepatitis livers overlapped with those of 60 HCCs, whereas those of hepatitis-negative LCBs diverged. The subsequent validation study on 68 LCBs identified recurrent mutations in TERT promoter, chromatin regulators (BAP1, PBRM1 and ARID2), a synapse organization gene (PCLO), IDH genes and KRAS. The frequencies of KRAS and IDHs mutations, which are associated with poor disease-free survival, were significantly higher in hepatitis-negative LCBs. This study reveals the strong impact of chronic hepatitis on the mutational landscape in liver cancer and the genetic diversity among LCBs.
本站所注明来源为"爱爱医"的文章,版权归作者与本站共同所有,非经授权不得转载。
本站所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们
联系zlzs@120.net,我们将立即进行删除处理
热点图文
-
AASLD2018研究进展丨慢乙肝患者治疗期间的肾脏安全管理
在新药取得成功之前,应用口服核苷(酸)类似物(NA)治疗慢性乙型肝炎(简称...[详细]
-
快讯丨TAF治疗4年的肝细胞癌发生率低于TDF
5月17日,在第十届全国疑难及重症肝病大会上,我国香港大学司徒伟基教授交流...[详细]