持续病毒学应答能降低慢性丙型肝炎死亡率
12月26号发表于《JAMA》杂志上的一项研究表明,在慢性丙型肝炎患者和肝纤维化患者中,基于干扰素疗法的持续病毒学应答能降低死亡率。
慢性丙型肝炎病毒(HCV)感染是肝硬化、肝细胞癌(HCC)及终末期肝病的重要风险因素。HCV相关的肝硬化及其并发症的发病率在未来几年预计将升高。根据文章的背景资料估计,目前慢性丙型肝炎发病率约为25%(350万人),并将在2030年增长到45%.
持续病毒应答是指停止所有抗病毒药物后24周不发生病毒血症。虽然SVR存在长期稳定性,但是支持其作为抗病毒治疗的替代终点的生存改善有关的数据尚不全面。展示其直接临床效果会更好的证明密集昂贵的抗病毒治疗的使用效果。
研究者探讨SVR的获得与否与慢性丙肝患者和肝纤维化患者的生存率是否有关。这项研究由欧洲和加拿大的5家三级医院完成,包括530位在1990年至2003年间接受干扰素治疗的慢性丙肝患者,收集肝纤维化和肝硬化的组织学证据。随访时间为2010年1月至2011年10月。随访时间中位数为8.4年,患者年龄基线中位数为48岁,369例(70%)为男性。
其中,192例(36%)获得SVR;13例获得SVR和100例未获得SVR的患者死亡。在进一步分析中研究者发现,SVR与全因死亡及肝脏相关的死亡率和移植率降低有关。其他基线因素包括衰老、HCV基因3型感染、糖尿病、酗酒,均与全因死亡密切相关。在未获得SVR的100例死亡患者中,70例患者死因与肝脏有关,15例与肝脏无关,15例未知。
肝脏相关的死亡或移植的10年累计发病率中,获得SVR的为1.9%,未获得的为27.4%.10年后,HCC的累计增长率,获得SVR的为5.1%,未获得的为21.8%.10年累积肝功能衰竭率,获得SVR的为2.1%,未获得的为29.9%.
在国际化多中心长期随访研究中,SVR与长期总体生存率相关。获得SVR与未获得的患者相比,各种原因的死亡率低4倍。长期随访研究表明,获得SVR慢性丙肝、肝纤维化和肝硬化患者死亡率降低。此外,研究者能够进一步建立和量化SVR患者肝癌、肝功能刷街以及肝脏相关的死亡率和移植率。
Sustained virological response linked with improved survival for patients with chronic HCV infection
Among patients with chronic hepatitis C virus infection and advanced hepatic fibrosis (development of excess fibrous connective tissue), sustained virological response (SVR) to interferon-based treatment was associated with a lower risk of all-cause mortality compared with patients without SVR, according to a study in the December 26 issue of JAMA.
"Chronic hepatitis C virus (HCV) infection is a major cause of cirrhosis, hepatocellular carcinoma (HCC), and end-stage liver disease. The incidence of HCV-related cirrhosis and its complications is expected to increase in upcoming years. Davis et al estimated that currently 25 percent of the approximately 3.5 million U.S. patients with chronic HCV infection have cirrhosis and that the proportion of patients with cirrhosis is likely to increase up to 45 percent by 2030," according to background information in the article.
"Sustained virological response is defined as absence of viremia [the presence of a virus in the blood] 24 weeks after cessation of all antiviral medication. Although SVR has long-term durability, data on the relationship with improved survival to support its use as a surrogate end point of antiviral therapy is scarce. Demonstrating direct clinical benefits would better justify the use of intensive and costly antiviral therapy …" the authors write.
Adriaan J. van der Meer, M.D., of Erasmus MC University Medical Center, Rotterdam, the Netherlands and colleagues conducted a study to examine whether achievement of SVR vs. without SVR is associated with a prolonged overall survival in patients with chronic HCV infection and advanced hepatic fibrosis. The study, conducted at five tertiary care hospitals in Europe and Canada, included 530 patients with chronic HCV infection who started an interferon-based treatment regimen between 1990 and 2003, following histological proof of advanced hepatic fibrosis or cirrhosis. Complete follow-up ranged between January 2010 and October 2011. The patients were followed up for a median (midpoint) of 8.4 years. The baseline median age was 48 years and 369 patients (70 percent) were men.
There were 192 patients (36 percent) who achieved SVR; 13 patients with SVR and 100 without SVR died (10-year cumulative all-cause mortality rate, 8.9 percent with SVR and 26.0 percent without SVR). In further analysis, the researchers found that SVR was associated with a reduced risk of all-cause mortality and liver-related mortality or transplantation. Other baseline factors significantly associated with all-cause mortality included older age, HCV genotype 3 infection, presence of diabetes, and a history of severe alcohol use. Of the 100 deaths in patients without SVR, the cause was liver-related in 70 patients (70 percent), not liver-related in 15 percent of patients, and unknown in another 15 percent.
The 10-year cumulative incidence rate of liver-related mortality or transplantation was 1.9 percent with SVR and 27.4 percent without SVR. After 10 years, the cumulative occurrence of HCC was 5.1 percent in patients with SVR and 21.8 percent in patients without SVR. The 10-year cumulative liver failure rate was 2.1 percent in patients with SVR vs. 29.9 percent in patients without SVR.
"In our international, multicenter, long-term follow-up study, SVR was associated with prolonged overall survival. The risk of all-cause mortality was almost 4-fold lower in patients with SVR compared with patients without SVR. Our study with a long follow-up duration demonstrated a lower risk for all-cause mortality in patients with chronic HCV infection and advanced hepatic fibrosis who achieved SVR. In addition, we were able to further establish and quantify the risk reduction of HCC, liver failure, and liver-related mortality or liver transplantation in patients with SVR," the authors conclude.
(JAMA. 2012;308(24):2584-2593; Available pre-embargo to the media athttp://media.jamanetwork.com)
本站所注明来源为"爱爱医"的文章,版权归作者与本站共同所有,非经授权不得转载。
本站所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,不希望被转载的媒体或个人可与我们
联系zlzs@120.net,我们将立即进行删除处理
热点图文
-
AASLD2018研究进展丨慢乙肝患者治疗期间的肾脏安全管理
在新药取得成功之前,应用口服核苷(酸)类似物(NA)治疗慢性乙型肝炎(简称...[详细]
-
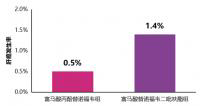
快讯丨TAF治疗4年的肝细胞癌发生率低于TDF
5月17日,在第十届全国疑难及重症肝病大会上,我国香港大学司徒伟基教授交流...[详细]